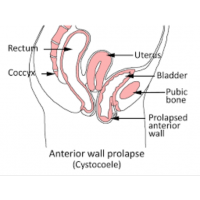
Bladder Prolapse
Diagram copyright Sue Croft Physiotherapist and used with permission
Bladder Prolapse
Bladder prolapse, also known as a cystocele or an anterior vaginal wall prolapse, occurs when the bladder pushes into the front wall of the vagina and is the most common form of pelvic organ prolapse due to there being less muscular support at the front of the pelvic floor.
Many women develop mild prolapse (particularly after pregnancy) and are unaware that they have it, this is termed non-symptomatic and it may never bother you. Some women can have a mild prolapse and feel very symptomatic.
Prolapses (uterus, bladder, bowel) are generally given grades or stages based on how far the organ has moved down or into the vagina from its original position.
There are, however, different opinions as to whether we should use these terms as they are slightly arbitary and what is 'normal' has yet to be properly established. As mentioned, some women can have a prolapse and be unaware of it, others are very aware. For many, these differences in awareness can fluctuate throughout the day as well, depending on what you have been doing. A 'grade 2' prolapse may measure at grade 3 by the end of the day and back again after a rest.
It is often best to go by symptoms, learn what makes you symptomatic and develop strategies to help manage the symptoms. See below for some ideas on this.
What causes a bladder prolapse?
It is commonly believed that pelvic organ prolapses are due to pelvic floor muscle weakness. This is a contributing factor but prolapse usually occurs due to a combination of factors, and some women are more prone to developing prolapse than others.
Causes:
- Fascial / elastic tissue damage - this can be torn or stretched.
- Pelvic floor muscle damage - weakened or torn (avulsed on one or both sides)
- A combination of both
What weakens the pelvic floor?
Symptoms:
- bulging felt in vagina or near the entrance, especially the front wall if it is a bladder prolapse.
- bulge seen at vaginal entrance or beyond
- heaviness in vagina especially after exercising, lifting or by the end of the day
- poor urine flow
- difficulty voiding (urinating)
- urinary urgency and / or freqency
- SUI = stress urinary incontinence ( although a bladder prolapse can mask SUI as it can kink the urethra and prevent leaks)
- constipation, straining to pass a bowel motion (the bladder may be pushing back towards the rectum)
- painful penetrative sex
- low back pain
What are the risk factors for a bladder prolapse?
- pregnancy
- vaginal birth
- instrumental birth - particularly forceps
- a third or fourth degree tear during childbirth
- long second stage (pushing ) of delivery >2 hours
- history of constipation (straining to pass bowel motions)
- obesity
- repeated heavy lifting
- family history of prolapse or hernias - may indicate poorer quality of connective tissue
- high impact exercise
- hypermobility ( as per the Beighton scale)
You can develop prolapse even if you have never been pregnant or if you have had a caesarean birth - if other risk factors are present.
Or you may have a number of risk factors and never develop prolapse or become symptomatic.
Some estimates suggest that half of all women who have had more than one child have some degree of prolapse, although only 10-20% experience symptoms that lead them to seek help.
Treatments for a bladder prolapse
- Lifestyle changes aimed at reducing pressures on the pelvic organs, pelvic floor and supporting elastic tissues:
- strengthening the pelvic floor muscles
- losing weight
- avoiding /managing constipation
- learning how to exercise correctly to avoid overloading the pelvic floor. This does not mean giving up exercise
and many women can continue to run and lift weights quite happily with a prolapse. - Pessaries are another conservative option that your physiotherapist or doctor may suggest. These are silicone devices of varying shape which are inserted into the vagina to provide support for the pelvic organs. They need to be properly fitted and you can be taught how to self-manage by inserting and removing when you need to use it.
- Surgical repair is suggested for more severe cases which have not responded to conservative measures and if the prolapse remains symptomatic.
It is always best to trial conservative treatment as desrcibed above first
URETHROCELE
Occurs when the urethra prolapses downwards into the vagina. It can happen by itself or along with a bladder prolapse. If this happanes it is alled a cystourethrocele. It can be managed in much the same way as above. Often a pessary will help to support the tissues.