Pelvic Organ Prolapse
Pelvic Organ Prolapse
A pelvic organ prolapse occurs when one of the pelvic orgnas descends from its normal position and presess against the wall of the vagina, or bulges into the vagina.
The term prolapse comes from the latin word prolapsus which translates to "a slipping forth" and means a falling, slipping or downwards displacement of an organ.
According to the IUGA/ICS joint terminolgy report a POP or Pelvic Organ Prolapse is primarily a definition of anatomical change.
There are several grades or stages of prolapse.
These are systems used to explain the degree to which the organ is descending and are measured in relation to the hymen - which is approximately at the entrance to your vagina.
You may have been told you have stage or grade 1, 2, 3 or 4 prolapse. The stage and grade are slightly different - and just mean that whoever has assessed you is either using the Baden-Walker scale (grade) or the POP-Q (stage) system of measuring how far down the organ has descended in relation to the hymen.
Whilst the higher the degree, the greater the prolapse, or more out of position the organ is, the main thing to focus on is symptoms.
You may have a stage 2 or 3 prolapse and be relatively symptom free.
Some women have a stage 1 prolapse and feel quite symptomatic.
It is all relative and very individual. So it isn't always helpful to focus on the degree, stage or grade and some of the language used by health professionals around prolapse can be quite alarming for you when you first hear it.
My main advice is don't panic, become informed and find a health professional with experience in managing prolapse to help guide you through the best way for you to manage yours.
What causes pelvic organ prolapse?
It is commonly believed that prolapse is due to pelvic floor muscle weakness. This is a contributing factor but prolapse usually occurs due to a combination of factors, and some women are more prone to developing prolapse than others.
Causes:
- Fascial / elastic tissue damage - this can be torn or stretched
- Pelvic floor muscle damage - weakened or torn (avulsed on one or both sides)
- A combination of both
- Check what weakens the pelvic floor
Symptoms:
- bulging felt in vagina or near the entrance
- bulge seen at vaginal entrance or beyond
- heaviness in vagina especially after exercising, lifting or by the end of the day
- poor urine flow
- difficulty voiding (urinating)
- urinary urgency and / or freqency
- SUI = stress urinary incontinence (although a bladder prolapse can mask SUI as it can kink the urethra and prevent leaks)
- constipation, straining to pass a bowel motion, difficulty wiping clean after a bowel motion, post defecation leaks
- painful penetrative sex
- low back pain
What are the risk factors for a prolapse?
- pregnancy
- vaginal birth
- instrumental birth - particularly forceps
- a third or fourth degree tear during childbirth
- long second stage (pushing ) of delivery >2 hours
- history of constipation
- obesity
- repeated heavy lifting
- family history of prolapse or hernias - may indicate poorer quality of connective tissue
- high impact exercise
- hypermobility (as per the Beighton scale)
You can develop prolapse even if you have never been pregnant or if you have had a caesarean birth - if other risk factors are present.
Or you may have a number of risk factors and never develop prolapse or become symptomatic.
Some estimates suggest that half of all women who have had more than one child have some degree of prolapse, although only 10-20% experience symptoms that lead them to seek help.
Types of Prolapse
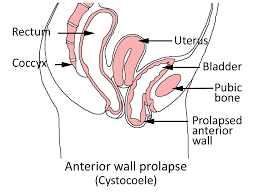
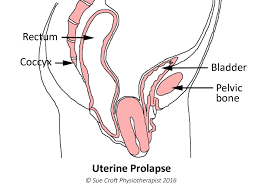
All diagrams are courtesy of Sue Croft Physiotherapist. They are from her books Pelvic Floor Essentials and Pelvic Floor Recovery
Copyright belongs to her and we thank her for allowing us to use them here.
1. BLADDER : previously called a cystocele, now more commonly called anterior wall descent or prolapse
This occurs when the bladder pushes into the front wall of the vagina and is the most common form of pelvic organ prolapse due to there being less muscular support at the front of the pelvic floor.
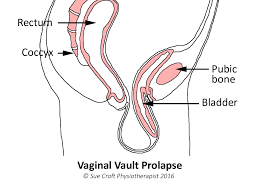
2. UTERINE and VAGINAL VAULT
Occurs when the uterus slides down the vagina. It can be felt as the cervix sitting lower than it should in the vagina. Women with a retroverted uterus are more prone to it prolapsing purely due to the mechanics.
The uterus in the first diagram is protruding from the vaginal entrance. For many women it will remain inside the vagina but sitting very low.
The second diagram shows the vaginal vault prolapsing. The vaginal vault is the top of the vagina that is left after a hysterectomy (removal of the uterus) and this can prolapse even though the uterus has been removed.
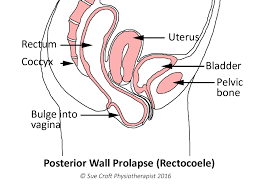
3. RECTUM or BOWEL: previously called a rectocele, now more commonly called a posterior wall descent or prolapse
This occurs when the rectum pushes into the back wall of the vagina, creating a pocket which can make passing a bowel motion (defecating) difficult and give the sensation of never fully emptying the bowel.
4. URETHROCELE
The urethra is the tube you wee through and it can prolapse downwards, sometimes without the bladder also prolapsing.
5. ENTEROCELE
Part of the small intestine descends behind the uterus between the rectum and the uterus.
6. RECTAL PROLAPSE : It is important to note that a rectal prolapse is NOT the same as a
rectocele or prolapse of the rectum into the vagina
A rectal prolapse occurs when the internal lining of the rectum decends down and protrudes from the rectum itself (via the anus or back passage)
It usually involves a degree of intussusception which is much like imagining your rectum is lined with a sock and the sock has lost its elasticity and has fallen down. This may require surgery but a mild prolapse can be managed with the help of your health professionals.
Treatments for prolapse
1. Lifestyle changes aimed at reducing pressures on the pelvic organs, pelvic floor and supporting
elastic tissues:
- strengthening the pelvic floor muscles
- losing weight
- avoiding /managing constipation
- learning how to exercise correctly to avoid overloading the pelvic floor. This does not mean giving up exercise and many women can continue to run and lift weights quite happily with a prolapse.
2. Pessaries are another conservative option that your physiotherapist or doctor may suggest. These are
silicone devices of varying shape which are inserted into the vagina to provide support for the pelvic
organs. They need to be properly fitted and you can be taught how to self-manage by inserting and removing when you need to use it.
3. Surgical repair is suggested for more severe cases which have not responded to conservative
measures and if the prolapse remains symptomatic.
Can I reverse an existing prolapse with pelvic floor exercises? Can I prevent a prolapse from happening?
Pelvic Floor Muscle training (PFMT) is considered the first choice of treatment for pelvic organ prolapse
- The multi-centre POPPY trial showed that pelvic floor muscle training can be effective in the improvement of prolapse symptoms.
- The updated Cochrane Review in 2011 also concluded there is a positive effect of pelvic floor muscle training in reducing prolapse stage and symptoms.
- Research from Norway demonstrates that pelvic floor muscle training (PFMT) improves prolapse severity. After 6 months, women in the study's PFMT group had significantly greater upwards lift of the bladder and rectum, compared with women in the control group. They also had reduced prolapse symptoms and greater improvement in pelvic floor muscle strength and endurance. (Braekken 2010)
- Read more about how to exercise the pelvic floor muscles correctly.
Can a pelvic floor exerciser help with my prolapse?
Pelvic floor or kegel exercisers can assist if you want to strengthen your pelvic floor, which is a recommended part of conservative management of pelvic organ prolapse. They can also provide excellent biofeedback as to how well you are doing your exercises, how you are progressing and providing an increasing challenge to your muscles.
Some vaginal weights are not suitable for use with a prolapse, as the prolapse may prevent correct positioning of the weight.
However if the prolapse is mild, vaginal cones such as Aquaflex or single weights like Teneo Uno can be used.
Biofeedback devices like Perifit can also be used if the prolapse allows you to insert them. Sometimes if the prolapse is sitting at the vaginal opening it can be difficult to get a device to sit correctly within the vagina.
The material presented here is intended as an information source only. The information is provided solely on the basis that readers will be responsible for making their own assessment of the matters presented herein and are advised to verify all relevant representations, statements and information. The information should not be considered complete and should not be used in place of the advice of a health care provider. Pelvic Floor Exercise does not accept liability to any person for the information or advice provided , or for loss or damages incurred as a result of reliance upon the material contained herein.
©Pelvic Floor Exercise all rights reserved